Complex Caring: The Challenge of TB-HIV Co-infection
A Long Road to the TB Clinic
 When Quan began his long series of visits to his primary care provider and emergency departments, co-infection with TB and HIV was the last thing on his mind. He had been in a car accident and had seen his primary care physician about a resulting injury. While recovering from the accident, he noticed a painful swelling under his arm. His doctor treated him for an abscess and infection of the lymph nodes in his armpit, but this didn’t bring him relief. On two occasions he went to the local emergency department with hot, painful swelling. He had a reaction to the antibiotic that was prescribed and returned to the emergency department with a spreading rash. When the swelling persisted for several weeks, his doctor ordered an aspiration biopsy of the affected lymph nodes.
When Quan began his long series of visits to his primary care provider and emergency departments, co-infection with TB and HIV was the last thing on his mind. He had been in a car accident and had seen his primary care physician about a resulting injury. While recovering from the accident, he noticed a painful swelling under his arm. His doctor treated him for an abscess and infection of the lymph nodes in his armpit, but this didn’t bring him relief. On two occasions he went to the local emergency department with hot, painful swelling. He had a reaction to the antibiotic that was prescribed and returned to the emergency department with a spreading rash. When the swelling persisted for several weeks, his doctor ordered an aspiration biopsy of the affected lymph nodes.
The result of this biopsy was the first of several shocks for Quan - he had TB of the lymph nodes. He was familiar with TB, having grown up in China, but did not think of himself as being at risk of developing the disease, living and working in a suburban setting in the U.S. Quan also had none of the classic symptoms of pulmonary TB and he had never heard of extra-pulmonary TB, that is, TB outside the lungs.
I first met Quan when his doctor referred him to the county TB clinic, where we began a routine evaluation. In addition to ordering a chest x-ray and collecting a sputum sample, we told him that it was our standard practice to draw blood to test for HIV infection. Quan said he didn’t need the test because he had been tested before and had only one intimate partner, who was HIV negative. Later in the conversation, he acknowledged that he did not know how long ago his partner was last tested. We explained to Quan that it was important that we know his HIV status so we could adjust our approach to his TB care if necessary; he then agreed to the test. We started him on a selfadministered regimen of 4 anti-TB drugs and scheduled a follow up appointment 2 weeks later. Meanwhile, we contacted his primary care physician for records of treatment for the swelling and abscess in his lymph nodes. By the time he left his first visit with us, Quan had started to absorb the reality of his TB diagnosis and seemed resolved to do what ever he could to speed along his recovery.
Quan’s follow-up visit brought the second big shock: the HIV counselor in our clinic told him that his test results showed that he was HIV-infected. She counseled him on how to prevent transmission and the importance of regular care by an HIV specialist. As his nurse case manager, I explained that his TB treatment would change. His regimen would be modified to avoid drug interactions with the therapy prescribed for HIV infection and the length of his TB treatment would be extended to 12 months. We emphasized the need to establish a relationship with an HIV specialist as soon as possible and offered to make a referral to an experienced HIV provider in the area.

We could see that the diagnosis and this onslaught of information were overwhelming to Quan. He said little, avoided meeting our gaze, and was close to tears. Eventually he expressed fear that he may have infected his partner with HIV. His partner Alvin was the only person he was really close to in the U.S. and was Quan’s sole support during the aftermath of the car accident. The HIV counselor gave Quan a list of places that Alvin could be tested and said he could come to her if he preferred. I asked Quan if he would like us to contact his partner, but he just shook his head to say no.
The Physical and Emotional Toll of Co-infection
As I began directly observed therapy (DOT) home visits, the physical and emotional toll of Quan’s dual diagnosis was unmistakable. The pain from his lymph nodes, swollen from TB infection, had grown so severe that he had been to the emergency department, where the nodes were aspirated. He was also beginning to develop symptoms of pulmonary TB, as his sputum culture results would confirm. In addition, Quan’s long-time doctor had suggested that he find another primary care physician, one who was qualified to treat HIV; that left Quan despondent about being separated from the provider he knew best, just when he was grappling with two potentially devastating illnesses.
As he recounted his discussion with his former doctor, I saw how the stigma attached to his diagnoses affected Quan’s emotions. TB and HIV were more than simply physical disorders, one an acute condition of which he could be cured, and the other a chronic infection that could be managed with medication; each also carries a heavy emotional burden. He thought of the diseases as representing something about the individuals who had them. He expressed this perception by contrasting “normal people,” or people without TB or HIV, to people “like him,” those who had one disease or the other. Therefore, in Quan’s mind, his previous primary care provider was an appropriate doctor for “normal” people, but not for people “like him.” He also expressed fears that he could not return to China to visit his family, or even inform his family about his health challenges, because his diagnoses would bring shame on the family. Because of the stigma he perceived surrounding everything connected to HIV, including HIV clinics, Quan found the processes of locating an HIV specialist and investigating what HIV care would be covered under his insurance extremely stressful.
Most distressing of all, was the knowledge that his partner Alvin was found to be HIV infected as well. As the couple discussed their diagnoses, Alvin revealed for the first time that a previous partner had died of AIDS. Quan went from feeling overwhelming guilt - believing that he was responsible for his partner’s infection, to a suspicion that Alvin had known or suspected he was HIV infected for several years and had not shared this with him.
The tension between them was obvious the first time I visited their home. Alvin immediately began talking: describing Quan’s physical state, his own need to be evaluated for TB disease in light of his HIV infection, and their difficulties finding an HIV provider with whom he was satisfied. In contrast, Quan was extremely withdrawn. He was so unresponsive that I wondered if he was having trouble understanding my English, although language had never been a barrier before. I was concerned that Quan was increasingly despondent and offered to refer him to a mental health provider, but he adamantly rejected the idea. I left the house worried about Quan’s deteriorating health and emotional state and wondering if his relationship with Alvin could survive the dual strains of his illness and their shared HIV diagnosis.
Over the next several weeks, Quan struggled with increasingly severe symptoms of TB disease. The TB clinic doctors explained that he was experiencing Immune Reconstitution Inflammatory Syndrome, or IRIS, in which some patients beginning TB treatment experience more severe symptoms as a result of heightened inflammatory response to TB. IRIS is not uncommon in patients co-infected with HIV and TB, and can occur even in TB patients whose immune systems are not affected by HIV. My relationship with Quan deepened as we worked together to manage symptoms associated with IRIS, treated the abscess under his arm, and coordinated appointments with his new HIV physician. Quan’s emotional health was equally precarious. In contrast to his earlier resolve to be cured of TB, he seemed now to feel hopeless. More than once, the doctors offered to refer him to a mental health provider, but he always refused. We were all concerned, but as his physical health gradually improved, so too did his spirits. Alvin became my patient as well, since he was given a diagnosis of TB after being evaluated at our clinic. Working in consultation with his HIV provider, the clinic doctors prescribed an adjusted 4-drug regimen for him, administered by directly observed therapy (DOT).
Getting in Touch with My Feelings
 Visiting them regularly for DOT in their house I saw their relationship gradually recover; Now, they would both greet me at the door and chat amiably during the visit. As we began settling into a regular DOT schedule and I was no longer totally absorbed in responding to Quan’s health crises, I had time to reflect on the complexity of providing care to a couple. Each member had his own personality and health needs, and his own way of dealing with illness and the life-changing challenges of an HIV diagnosis. At times, I had the sense that Alvin over-dramatized his own health challenges or practical needs in order to keep attention focused on himself. Sometimes too, I felt that Alvin was unwilling for me to engage Quan in conversation outside his presence. I realized that I had to work to establish smoother communication patterns among Continued from page 2 Quan, Alvin, and their care team if we were to get through the remaining months of TB treatment ahead.
Visiting them regularly for DOT in their house I saw their relationship gradually recover; Now, they would both greet me at the door and chat amiably during the visit. As we began settling into a regular DOT schedule and I was no longer totally absorbed in responding to Quan’s health crises, I had time to reflect on the complexity of providing care to a couple. Each member had his own personality and health needs, and his own way of dealing with illness and the life-changing challenges of an HIV diagnosis. At times, I had the sense that Alvin over-dramatized his own health challenges or practical needs in order to keep attention focused on himself. Sometimes too, I felt that Alvin was unwilling for me to engage Quan in conversation outside his presence. I realized that I had to work to establish smoother communication patterns among Continued from page 2 Quan, Alvin, and their care team if we were to get through the remaining months of TB treatment ahead.
I could not deny that I had a stronger connection to Quan, especially because we had been through his struggle with IRIS together. I felt, too that he was particularly vulnerable as the younger partner in the couple and a recent immigrant with few important relationships other than Alvin. My empathy for him seemed natural and spontaneous.
At the same time, I knew that demonstrating empathy towards Alvin was part of my responsibility to him as a healthcare provider; if I didn’t establish a strong therapeutic relationship with him I would be less able to respond effectively if complications arose in the future. While I may not have spontaneously felt the same positive regard for Alvin that I did for Quan, I had the professional skills to develop a compassionate, healing attitude towards him. I drew on my training and years of experience to create a closer bond with him, consciously regulating my reactions to Alvin’s expression of worry about his medications and his comments about Quan’s care so that I listened more patiently and responded more directly to Alvin’s concerns. As I became more deliberate about showing interest in Alvin and sympathy with him, I realized that he in turn began to express himself more calmly and was less demanding of my time.
Teamwork
In my effort to build a stronger therapeutic relationship with both of them I had the support of Olivia, an experienced outreach worker who shared responsibility with me for DOT visits to Quan and Alvin’s home. She met both of them at about the same point in their care and perhaps because of this, her relationships with each developed more equally than mine. Olivia sensed that Alvin felt uncomfortable talking about his own fears in front of Quan, so when tensions were particularly high at home, she met with Alvin at a neighborhood coffee shop. Even when she had no solution to offer, Olivia took the time to listen and offer encouragement. Sometimes the encouragement came not so much from her words, but from her positive outlook and an attitude that conveyed her confidence in their treatment and progress. She asked them both about their interests, eventually exchanging favorite recipes with Quan and chatting with Alvin’s mother who came to visit over the holidays. Discussing their cases with Olivia and understanding how her perceptions of each man differed from mine helped me to gain perspective on my own attitudes towards both patients, so that I could better regulate my responses to them. She shared with me what she had learned about their personal interests, details that gave me a fuller understanding of each man beyond TB and HIV and provided the basis for casual conversation in their home.
I believe that when their treatment ended both men felt that ours had been a positive relationship; they continue to keep in touch through holiday cards and stop by the clinic to say hello every once in while. I think they are proud that they weathered the long period of illness, difficult diagnoses, and treatment together. I too, feel a sense of accomplishment about the relationships I was able to develop with each of them and the care that Olivia and I provided together.
Self-Awareness
In the case described in this issue, the nurse case manager was able to recognize that she had different emotional reactions to each of her two patients, foresee the possible negative consequences her feelings might pose to their care, and take steps to deal with her emotions in order to ensure positive outcomes for both men. She did so by practicing self-awareness (see definition). While self-awareness is mainly about how we view ourselves, it also effects how we deal with others and is an integral element necessary for understanding and improving the quality of healthcare services, including cultural competency.
Self-Awareness in Cultural Competency
Self-awareness is central to the development of cultural competency, because it contributes to the formation of attitudes that promote effective, respectful communication across cultures. Understanding our own unique emotional makeup and how it influences our thoughts as well as interactions with others helps us develop the ability to recognize and respond appropriately to the emotions, beliefs, norms, and values of others. The influence of self-awareness goes beyond interpersonal skills. It also contributes to perspectives and behaviors at the institutional level that promote responsiveness to culturally diverse communities and needs.
Definition of Self-Awareness
An understanding of how one is affected by events and personal interactions and conversely how one’s attitude and actions impact others (O’Connor, 2008).
By practicing self-awareness, we recognize our own feelings and perceptions and identify how they influence our reasoning, judgment, attitudes, and behaviors. At the same time, self-awareness is important for our interactions with others; the effects of our behaviors on others and their reactions to our behaviors give us a way to evaluate what we do and why. A recent review of the concept as applied to nursing describes self-awareness as the development of skills to respond to our environment in ways that are in keeping with our self-identified values and beliefs. With increased self-awareness, we learn to delay instinctive behaviors and instead use our insight either to make behavior changes, or knowingly choose specific behavioral responses (Eckroth-Bucher, 2010).
Self-awareness is part of a larger group of skills that constitute what is known as emotional intelligence (EI) (Goleman, 2004); (Bar-On, 2007); (Lopes, et al., 2004). EI refers to how we recognize, make sense of, and use emotion to strengthen the way we think and the way we interact with others. A leading definition describes it as the ability to “pay attention to, use, understand, and manage emotions [in ways that] serve [our ability to] adapt (Mayer, Salovey, & Caruso, 2008).” EI is increasingly recognized as an essential part of being a competent professional, influencing job performance (including patient outcomes) as well as job satisfaction, team dynamics, job retention, and burnout (Codier, Muneno, Franey, & Matsuura, 2010). It may be particularly important in nursing (Silva, Sorrell, & Sorrell, 1995), which requires exceptional interpersonal skills to be able to support individuals and families through crises and contribute to smoothly functioning care teams. EI is learned and can be developed progressively through a combination of training (Horton-Deutsch & Sherwood, 2008), and reflection on professional practice (Down, 2002).
Attitudes and values concerning healthcare related issues may be culturally specific to both patient and provider.
These issues include the individual’s:
• Autonomy to make decisions affecting his or her care
• Definitions of health, illness, and healthcare
• Family networks and understanding of family authority
• Understanding of gender roles in family decisionmaking and socializing
• Desired degree of acculturation into the dominant culture
Checklist for self-assessment of cultural and linguistic competence developed at the Center for Child and Human Development at Georgetown University (Goode, 1989, revised 2009)
Developing Self-Awareness
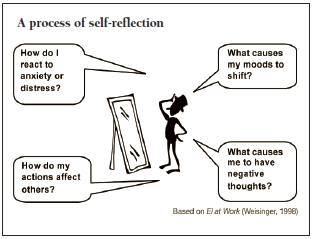
Whether it is developed through training, in-depth supervision, or self-study, self-awareness is an on-going process. Individuals can begin the process by reflecting on how much they practice self-awareness in their daily life.
References
Bar-On, R. (2007). The Bar-On model of emotional intelligence: A valid, robust and applicable EI model. Organisations & People, 14, 27-34.
Codier, E., Muneno, L., Franey, K., & Matsuura, F. (2010). Is emotional intelligence an important concept for nursing practice? J Psychiatr Ment Health Nurs, 17(10), 940-948.
Down, J. (2002). Therapeutic Nursing and Technology: Clinical Supervision and Reflective Practice in a Critical Care Setting. In D. Freshwater (Ed.), Therapeutic Nursing. Improving Patient Care through Self Awareness and Reflection. Thousand Oaks, CA: Sage Publications.
Eckroth-Bucher, M. (2010). Self-awareness: a review and analysis of a basic nursing concept. ANS Adv Nurs Sci, 33(4), 297-309.
Goleman, D. (2004). What makes a leader? Harvard Business Review, 82(1), 82-+.
Goode, T. (1989, revised 2009). Promoting Cultural and Linguistic Competency:Self-Assessment Checklist for Personnel Providing Primary Health Care Services. In E. National Center for Cultural Competence Georgetown University Center for Child & Human Development University Center for Excellence in Developmental Disabilities, Research & Service (Ed.).
Horton-Deutsch, S., & Sherwood, G. (2008). Reflection: an educational strategy to develop emotionally-competent nurse leaders. Journal of Nursing Management, 16(8), 946-954.
Lopes, P. N., Brackett, M. A., Nezlek, J. B., Schutz, A., Sellin, I., & Salovey, P. (2004). Emotional intelligence and social interaction. Pers Soc Psychol Bull, 30(8), 1018-1034.
Mayer, J. D., Salovey, P., & Caruso, D. R. (2008). Emotional intelligence: new ability or eclectic traits? Am Psychol, 63(6), 503-517.
O’Connor, M. (2008). The dimensions of leadership: a foundation for caring competency. Nurs Adm Q, 32(1), 21-26.
Silva, M. C., Sorrell, J. M., & Sorrell, C. D. (1995). From Carper’s patterns of knowing to ways of being: an ontological philosophical shift in nursing. ANS Adv Nurs Sci, 18(1), 1-13.
Weisinger, H. (1998). Emotional Intellegence at Work: the untapped edge for success. San Francisco: Jossey-Bass.
Psychosocial Aspects of HIV Diagnosis
 Over the past 25 years, effective treatment and improved systems of care have helped transform HIV infection into a manageable chronic disease for many people. Nevertheless, a diagnosis of HIV infection can be an emotionally overwhelming experience. Supportive services, such as basic health education, counseling about how and to whom to disclose HIV infection, and referrals for more on-going services if needed can help patients come to terms with their diagnosis. The common range of emotional reactions for a person to experience after hearing the diagnosis include shock, denial, anger, fear, grief, and sadness. A newly diagnosed person may experience some or all of these feelings over a period of time (Theuninck, Lake, & Gibson, 2010).
Over the past 25 years, effective treatment and improved systems of care have helped transform HIV infection into a manageable chronic disease for many people. Nevertheless, a diagnosis of HIV infection can be an emotionally overwhelming experience. Supportive services, such as basic health education, counseling about how and to whom to disclose HIV infection, and referrals for more on-going services if needed can help patients come to terms with their diagnosis. The common range of emotional reactions for a person to experience after hearing the diagnosis include shock, denial, anger, fear, grief, and sadness. A newly diagnosed person may experience some or all of these feelings over a period of time (Theuninck, Lake, & Gibson, 2010).
A person’s distress over an HIV diagnosis may go beyond these reactions and indicate a mood disorder, such as clinical depression; signs include severe distress that persists over 2 or more weeks, recurrent thoughts of death or suicide, a suicide attempt, and lack of affect or denial of any feelings about the diagnosis. These symptoms should be fully evaluated by a mental health professional.
Populations at elevated risk of acquiring HIV also tend to experience higher than normal rates of mood disorders (Perkins, et al., 1994). Diagnoses of mood disorders in HIV patients can be complicated by overlapping symptoms; for instance, weight loss, fatigue, and sleep disturbances may characterize both HIV infection and depression. In addition, medications may cause side effects that mimic symptoms of mood disorders, and co-occurring substance use may also be implicated in the mental health evaluation of newly diagnosed HIV patients. All of these factors should be addressed in a mental health evaluation.
Unrecognized, unaddressed mental health needs can affect HIV patients’ physical well-being, quality of life, coping mechanisms, self-care behaviors, and their ability to adhere to treatment regimens. Thus, adequate mental health care is an important dimension of quality HIV care (Aberg, et al., 2009). Mood disorder drug regimens can be successfully combined with antiretroviral therapy to suppress HIV, and psychotherapy, (individual, family, or group), is also effective in helping HIV patients achieve mental and physical well-being (Himelhoch, Moore, Treisman, & Gebo, 2004).
References
Aberg, J. A., Kaplan, J. E., Libman, H., Emmanuel, P., Anderson, J. R., Stone, V. E., et al. (2009). Primary Care Guidelines for the Management of Persons Infected with Human Immunodeficiency Virus: 2009 Update by the HIV Medicine Association of the Infectious Diseases Society of America. Clinical Infectious Diseases, 49(5), 651-681.
Himelhoch, S., Moore, R. D., Treisman, G., & Gebo, K. A. (2004). Does the presence of a current psychiatric disorder in AIDS patients affect the initiation of antiretroviral treatment and duration of therapy? Jaids-Journal of Acquired Immune Deficiency Syndromes, 37(4), 1457-1463.
Perkins, D., Stern, R., Golden, R., Murphy, C., Naftolowitz, D., & Evans, D. (1994). Mood disorders in HIV infection: prevalence and risk factors in a nonepicenter of the AIDS epidemic. Am J Psychiatry, 151(2), 233-236.
Theuninck, A. C., Lake, N., & Gibson, S. (2010). HIV-Related Posttraumatic Stress Disorder: Investigating the Traumatic Events. Aids Patient Care and Stds, 24(8), 485-491.
TB/HIV Co-Infection
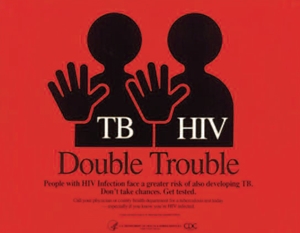 A patient with both HIV and TB infections requires special medical management since treatment for each disease must take into account the effect of the other. Globally, TB is the cause of death in approximately one-third of AIDS patients, and conversely, HIV disease is among the most important factors driving the global spread of TB. In the US, the HIV epidemic was implicated in the rapid rise in TB incidence in the 1980s-1990s. Over the past several years, the proportion of TB cases with HIV co-infection has remained at approximately 10% (Luetkemeyer, 2010). The presence of HIV disease complicates the diagnosis and treatment of both latent TB infection (LTBI) and active TB disease. For this reason, determination of HIV status is an important element in the evaluation of patients with known or suspected TB disease, and will influence recommendations concerning treatment for LTBI.
A patient with both HIV and TB infections requires special medical management since treatment for each disease must take into account the effect of the other. Globally, TB is the cause of death in approximately one-third of AIDS patients, and conversely, HIV disease is among the most important factors driving the global spread of TB. In the US, the HIV epidemic was implicated in the rapid rise in TB incidence in the 1980s-1990s. Over the past several years, the proportion of TB cases with HIV co-infection has remained at approximately 10% (Luetkemeyer, 2010). The presence of HIV disease complicates the diagnosis and treatment of both latent TB infection (LTBI) and active TB disease. For this reason, determination of HIV status is an important element in the evaluation of patients with known or suspected TB disease, and will influence recommendations concerning treatment for LTBI.
As the case highlighted in this issue illustrates, many patients are devastated to receive news of their positive HIV test results in addition to a diagnosis of TB disease. Multiple resources exist to help providers deliver HIV-related results in a compassionate manner that establishes the foundation for high-quality HIV care and treatment.*
In addition, the presence of HIV infection may make it more difficult to detect TB infection, especially in individuals with impaired immune systems (indicated by CD4-T cell counts below 200 cells per milliliter). In HIV-infected individuals, an induration of 5 mm or greater in response to a Tuberculin Skin Test (Mayer, et al.) is considered positive for TB infection, but in individuals with advanced HIV disease whose bodies have lost the abililty to react to the tuberculin, the TST result is often a false negative. Newer blood based assays for TB infection (IGRAs) are more effective at accurately detecting the presence of M. tuberculosis in HIV infected patients (CDC, 2010; Centers for Disease Control and Prevention, 2010).
HIV-infected individuals are at high risk of developing TB disease following infection, with a risk between 7 and 10% annually, compared to a lifetime risk of 5 – 10 % in those without HIV infection. People with HIV who are in contact with a person who has infectious TB disease should be treated for latent TB infection (LTBI) regardless of their TST test results even if they have received treatment for LTBI in the past. Intensified efforts to ensure that HIV patients complete LTBI treatment, including directly observed therapy, are warranted given the increased risk of the patient’s infection progressing to active TB disease and the potentially devastating effect of TB disease in HIV-infected individuals.
People who are in the early stages of HIV (CD4+ T-cell counts above 350 milliliters), present with TB much the same as other patients. However, patients with advanced HIV disease having more severe immune impairment, often have an atypical presentation of TB, including extrapulmonary (outside the lung) disease, with infections in the lymph nodes, pleura, nerve tissue and pericardium. In such cases usual diagnostic tools, such as sputum culture for M. tb, may be less effective than a doctor’s suspicion of TB in making an accurate diagnosis (Luetkemeyer, 2010). While the principles of TB treatment are essentially the same regardless of HIV infection, there are several important considerations in treatment of TB-HIV co-infection. The standard TB treatment may need to be extended to 9 months or more. More severely immuno-compromised patients (with CD4+ cell counts below 200/mm3) are at higher risk of developing acquired drug (rifampin) resistance. Therefore, current guidelines recommend that HIV patients receive daily, or 3x weekly therapy, not intermittent (Kaplan, et al., 2009). A more complex treatment issue concerns the interaction of TB drugs and antiretroviral medications (used to reduce HIV infection). In any case TB treatment should not be delayed, and, it is important to work closely with the patient’s HIV provider in order to determine adjustments that may be needed to treatment regimens and ensure that each patient is appropriately monitored (Centers for Disease Control and Prevention, 2007)
* Resources on how to deliver HIV test results include a recent DVD and discussion guide produced by the Region I Federal Training Centers Collaborative (FTCC): Region I Title X Family Planning Training Center; New England AIDS Education and Training Center; Sylvie Ratelle STD/HIV Prevention Training Center of New England; New England Addiction Technology Transfer Center; and the New Jersey Medical School Global TB Institute: http://www.famplan.org/Resources/hiv_aids.htm)
References
Centers for Disease Control and Prevention. (2007). Managing Drug Interactions in the Treatment of HIV-Related Tuberculosis. from http://www.cdc.gov/tb/publications/guidelines/TB_HIV_Drugs/default.htm
Centers for Disease Control and Prevention. (2010). Report of Expert Consultations on Rapid Molecular Testing to Detect Drug-Resistant Tuberculosis in the United States. from http://www.cdc.gov/tb/topic/Laboratory/rapidmoleculartesting/default.htm
Kaplan, J. E., Benson, C., Holmes, K. H., Brooks, J. T., Pau, A., & Masur, H. (2009). Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep, 58(RR- 4), 1-207; quiz CE201-204.
Luetkemeyer, A. F. (2010). Current issues in the diagnosis and management of tuberculosis and HIV coinfection in the United States. Top HIV Med, 18(4), 143-148.
Mayer, J. D., Goleman, D., Barrett, C., Gutstein, S., Boyatzis, R., Goldberg, E., et al. (2004). Leading by feel. Harvard Business Review, 82(1), 27-+.











